Topic 2
PTSI and you
In this section, we’ll learn about the connection between trauma and mental health, symptoms you might notice in your loved one if they’re dealing with trauma, and how your Family life might change when someone you love has a mental health challenge or condition.
Want to listen to this information? Play the audio track and follow along through the section as you listen!
(Narrator) As a young Family member of a Veteran, it may be helpful to understand the word “trauma” and some of the terms used when talking about mental health in the context of trauma.
When someone sees or experiences things that are deeply distressing, shocking or disturbing, like an accident or a crime, it can have a lasting emotional impact. This response is called trauma.
Trauma can happen after one event or multiple events.
These events can be extreme and even life-threatening, but may not always involve disaster or death. Things like discrimination or bullying can also lead to trauma.
Sometimes, people can have trauma by hearing or reading about certain situations or events.
Your loved one may or may not acknowledge that they are struggling or share the true extent of their struggles with you.
The important thing to remember is that not everyone will have trauma, even after experiencing the same event, and most who do will recover over time. But sometimes, even after a long time, people can struggle with its effects.
You may hear words like posttraumatic stress disorder (PTSD for short), posttraumatic stress injury (PTSI for short) or operational stress injury (OSI for short). These are all terms to describe a mental health injury related to trauma, but each means something different.
Talking about trauma can be difficult and confusing
Everyone is different. Two people can experience the same situation or event and only one may have trauma as a result. Most people who experience trauma will recover over time.
Sometimes, people can experience mental health challenges or conditions for a long time after traumatic events.
You may hear terms like posttraumatic stress injury, posttraumatic stress disorder or operational stress injury. These terms may come up when your loved one talks about their mental health.
On the other hand, you may not hear any of these terms, despite noticing that something is different with your loved one. There are many reasons for this — your loved one might not recognize the signs and symptoms or think they are experiencing a mental health challenge or condition, or they may want to protect you or worry about how you or others will respond if they admit they are having a tough time.









[Thomas walks back home. He hesitates for a moment before opening the door.]
(Mom): Thomas, you’re home late. Where were you?
(Thomas): I was doing homework with my friends at school.
[Thomas gently puts down his shoes and school bag. Dad is watching TV in another room.]
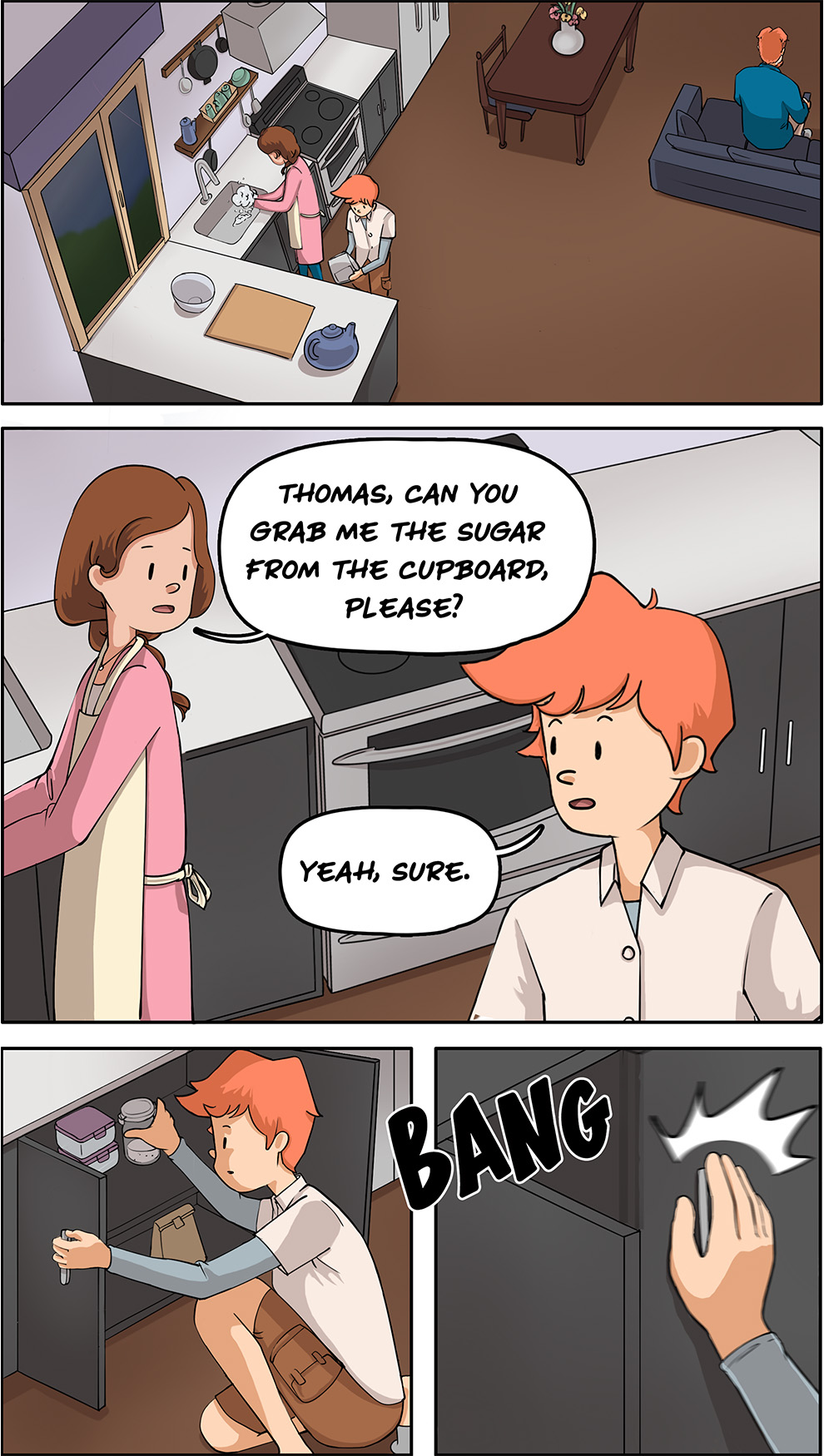
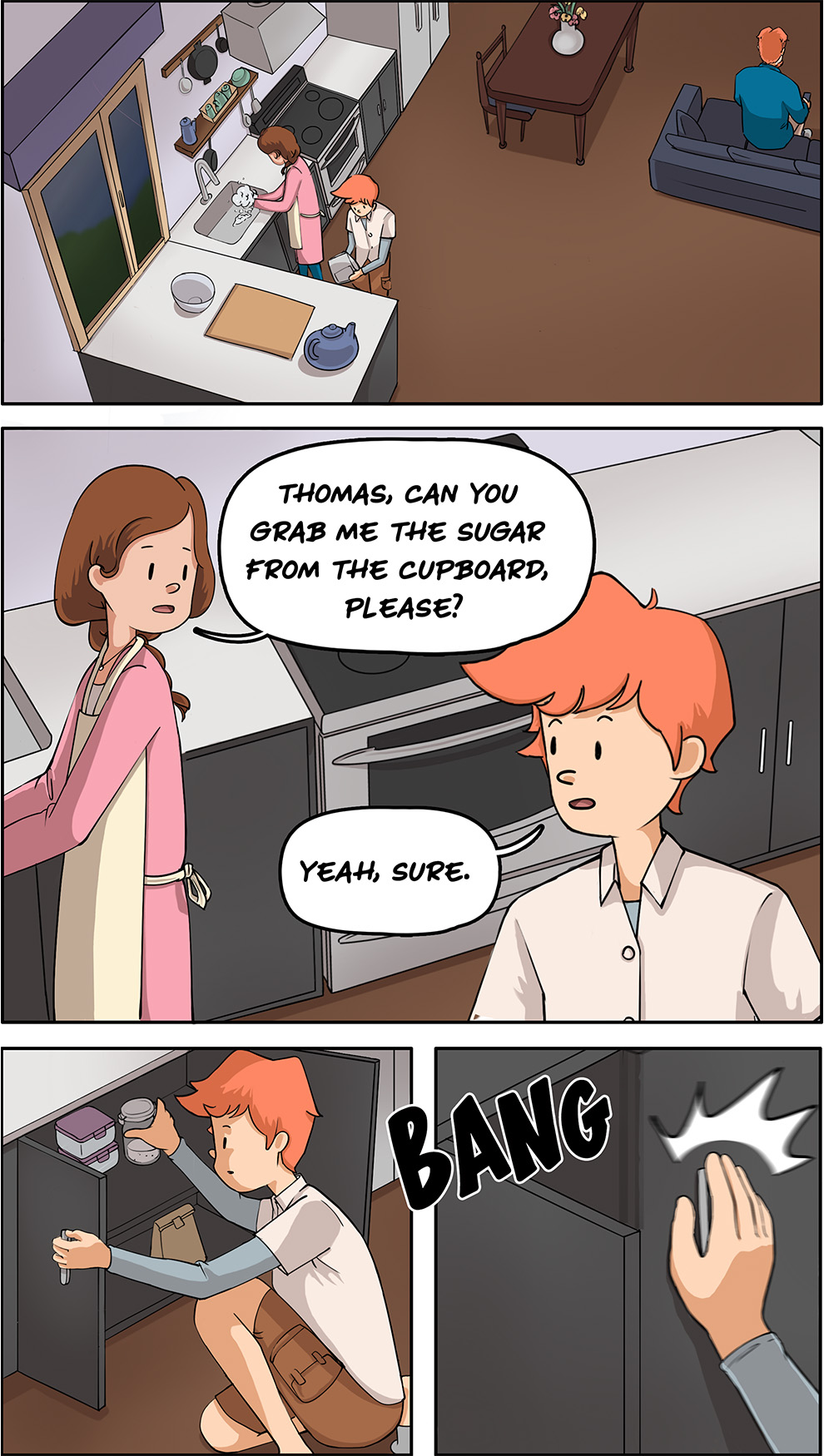
[Thomas and his mom are in the kitchen making a snack.]
(Mom): Thomas, can you grab me the sugar from the cupboard, please?
(Thomas): Yeah, sure.
[Thomas grabs the sugar from the cupboard. The cupboard door slams shut loudly: “bang.”]
Thomas cringes and looks over his shoulder towards Dad to check his reaction.
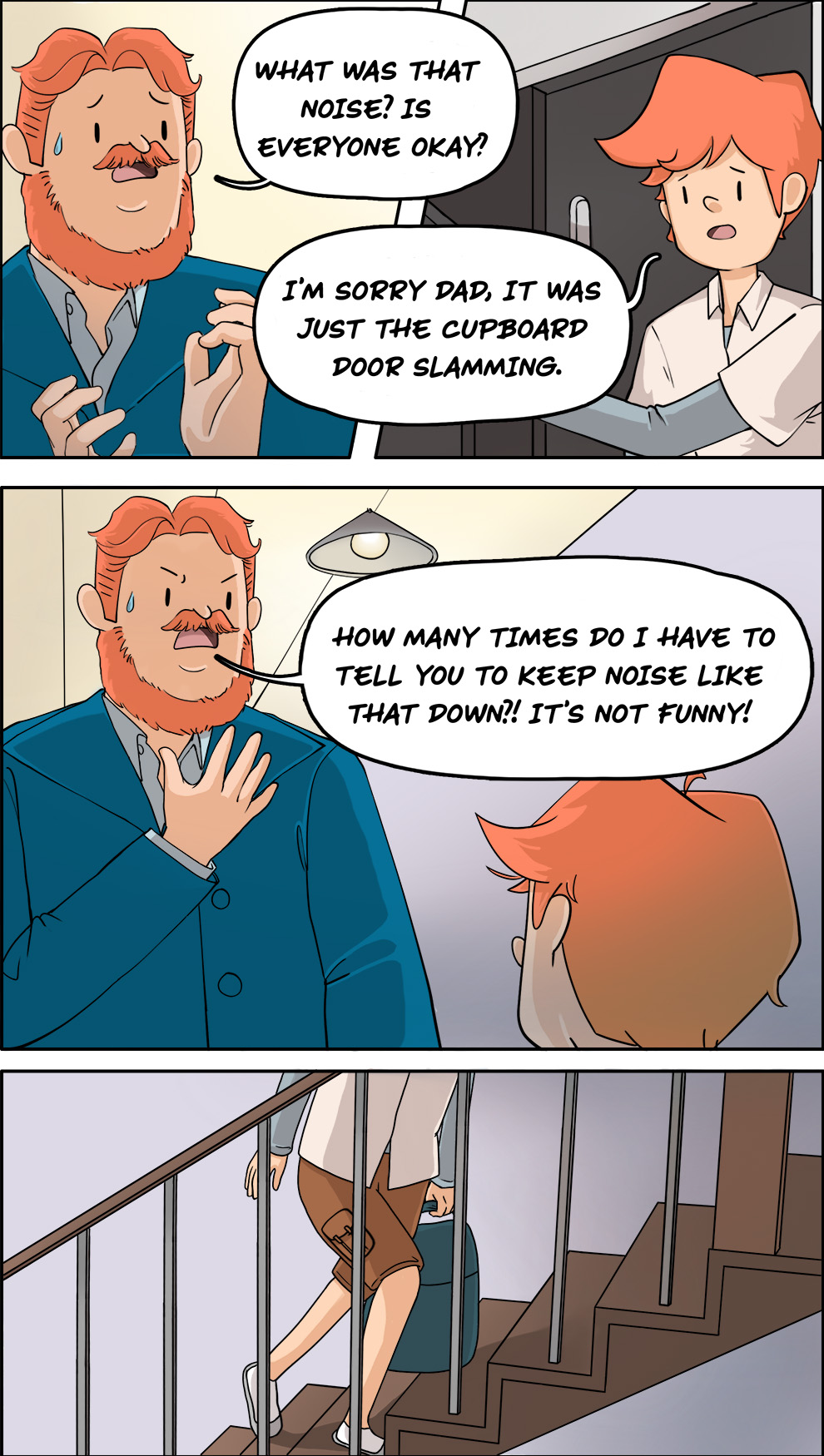
[Dad is startled and jumps up, ready to protect his Family. Dad runs into the kitchen.
(Dad): What was that noise? Is everyone okay?
(Thomas): I’m sorry Dad, it was just the cupboard door slamming.
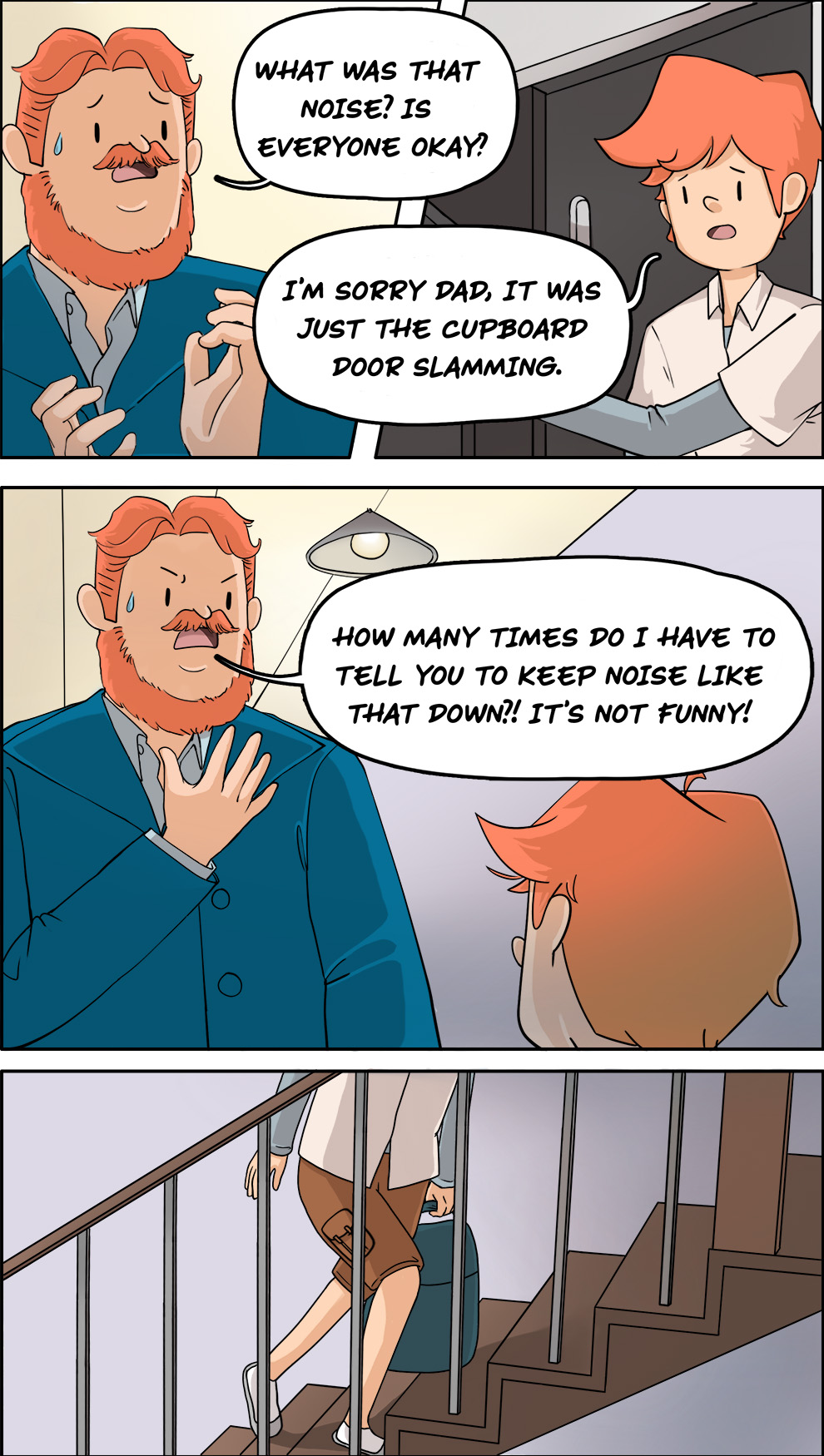
(Dad): How many times do I have to tell you to keep noise like that down?! It’s not funny!
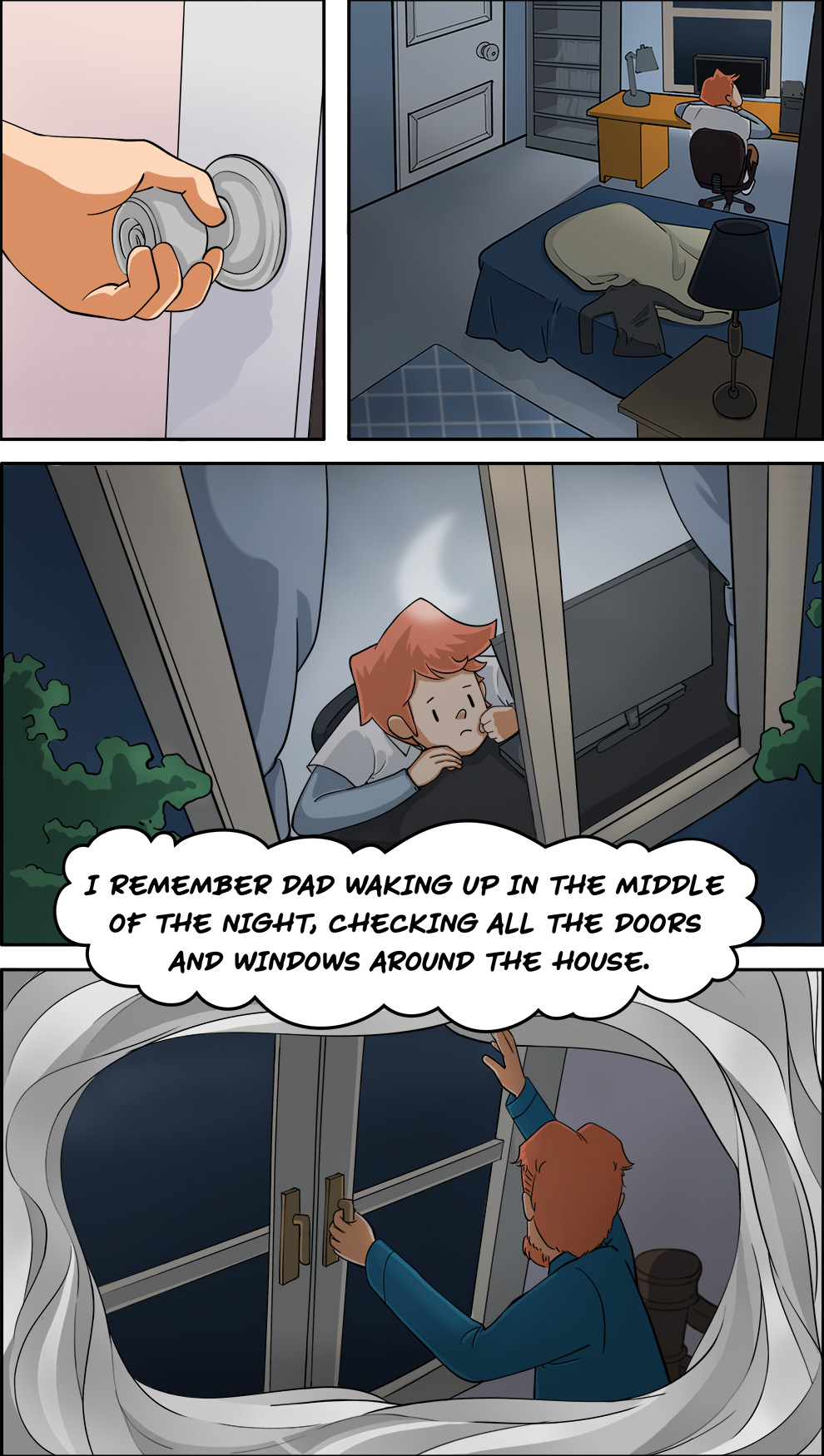
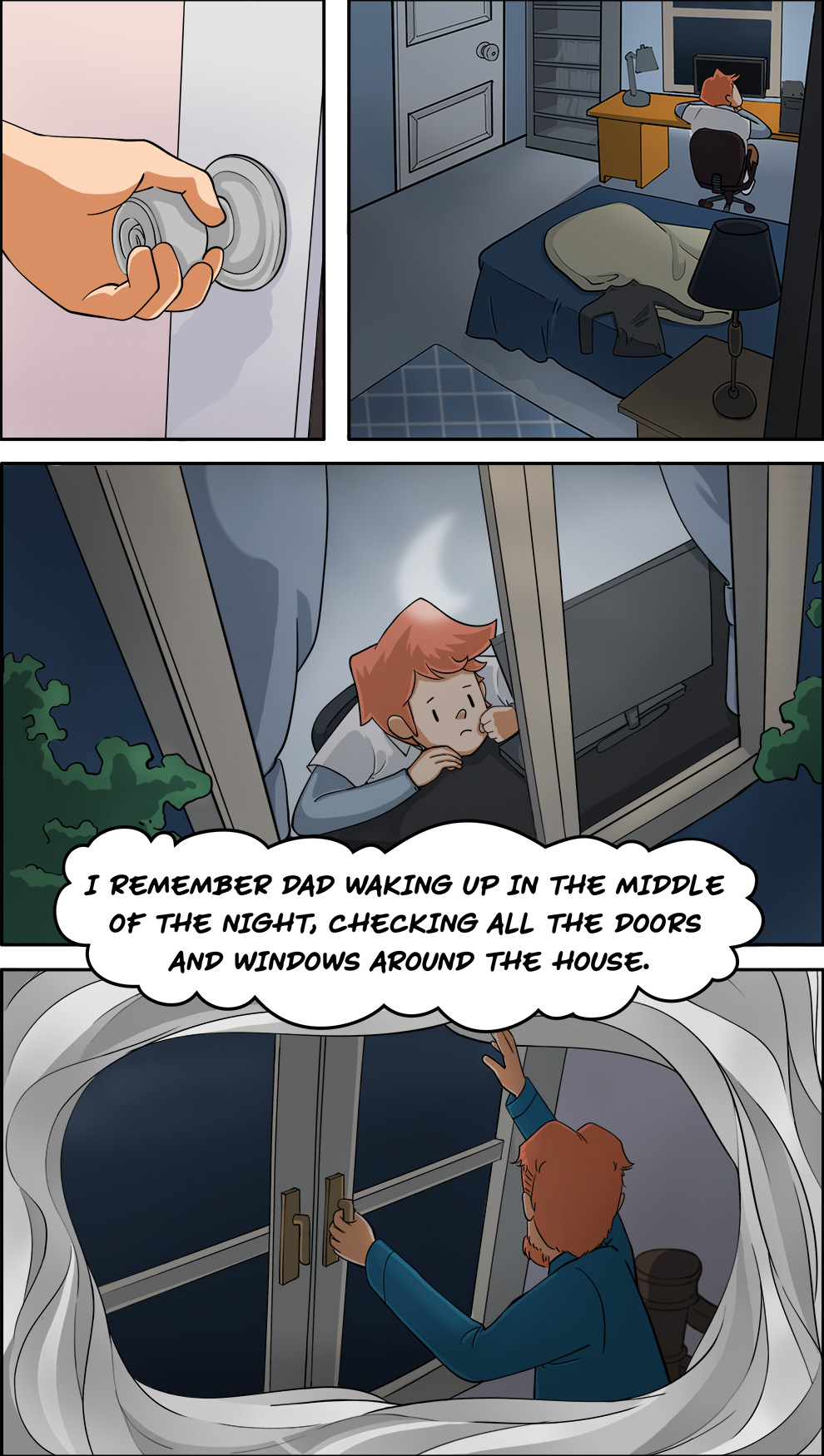
[Thomas goes to his room. He looks out of the window, thinking back to how Dad has changed.]
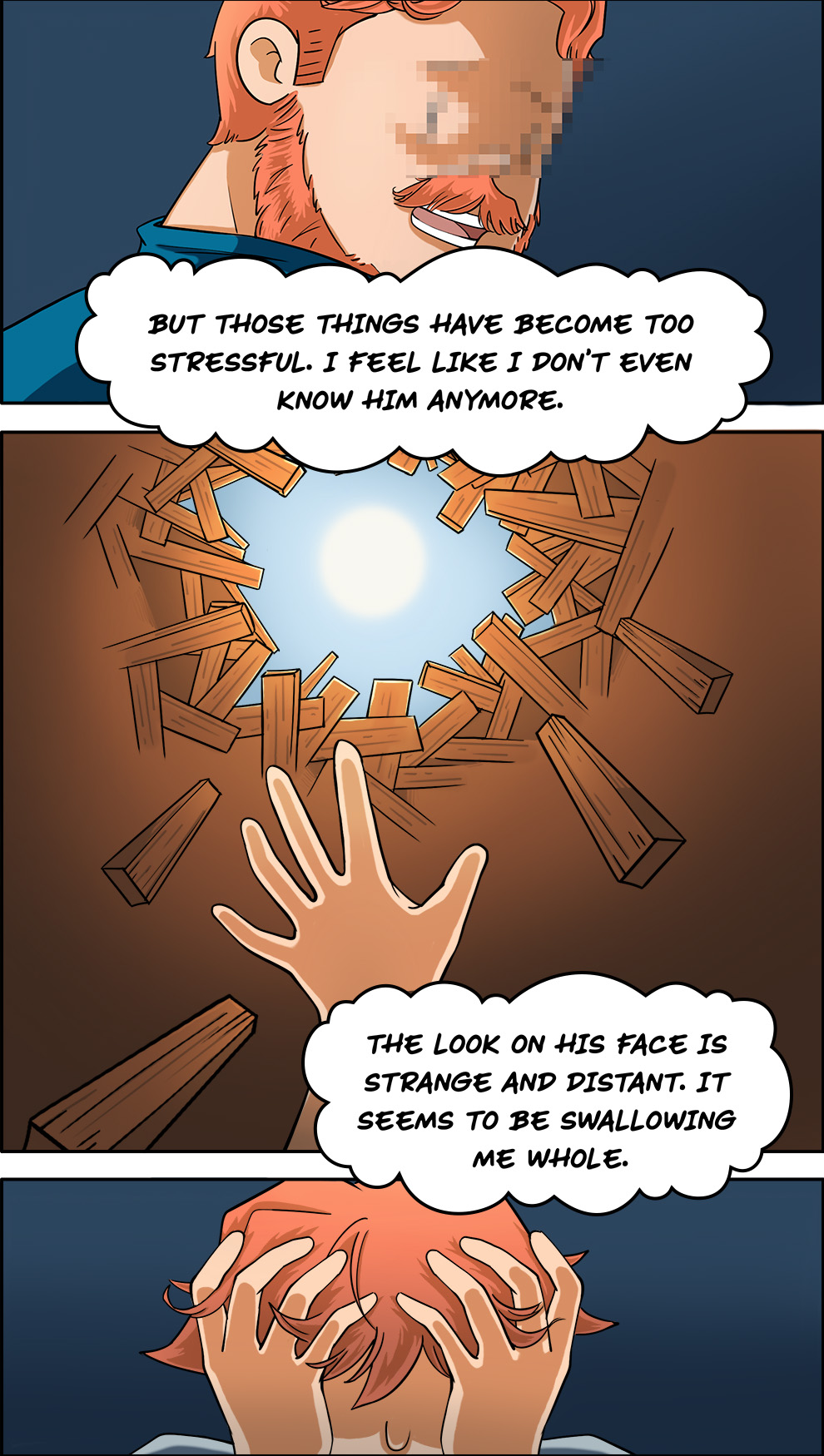
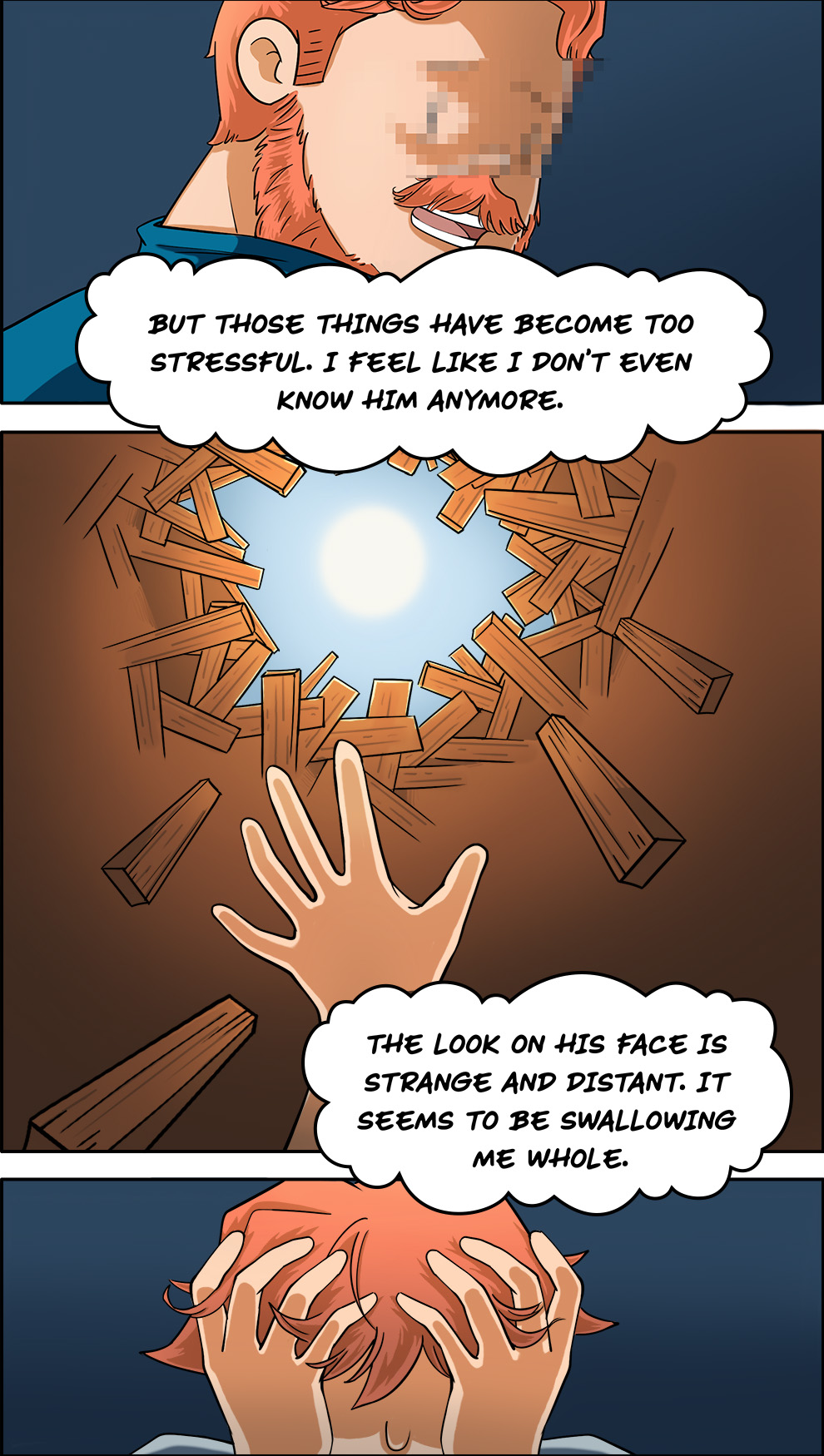
(Thomas): I remember Dad waking up in the middle of the night, checking all the doors and windows around the house. Sometimes he wakes up screaming and yelling from nightmares too. Mom’s started sleeping in a different room. We used to go to hockey games together and have picnics at the park, but those things have become too stressful. I feel like I don’t even know him anymore. The look on his face is strange and distant. It seems to be swallowing me whole.
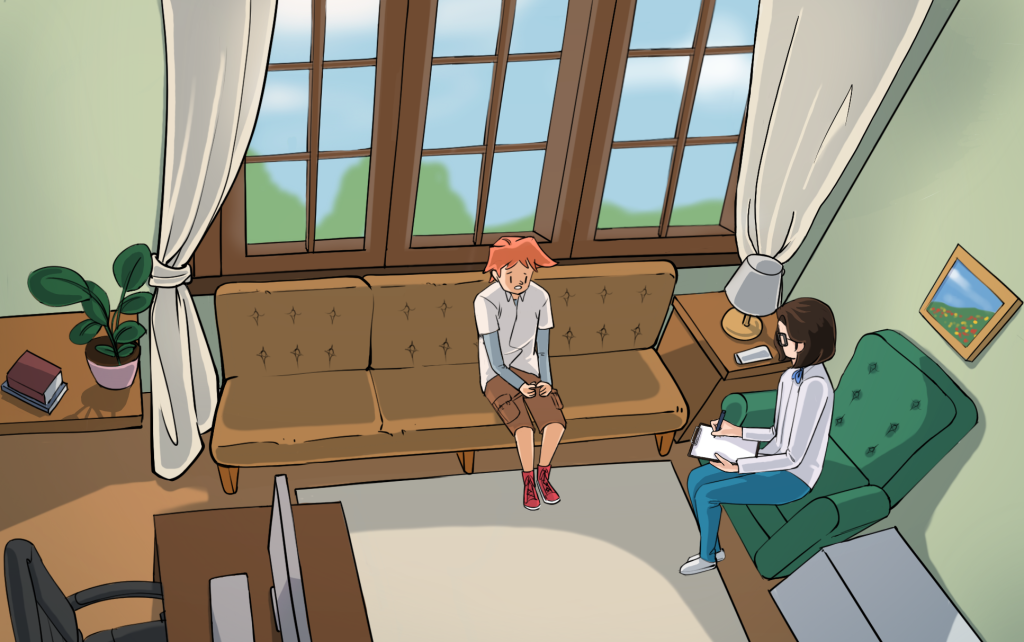
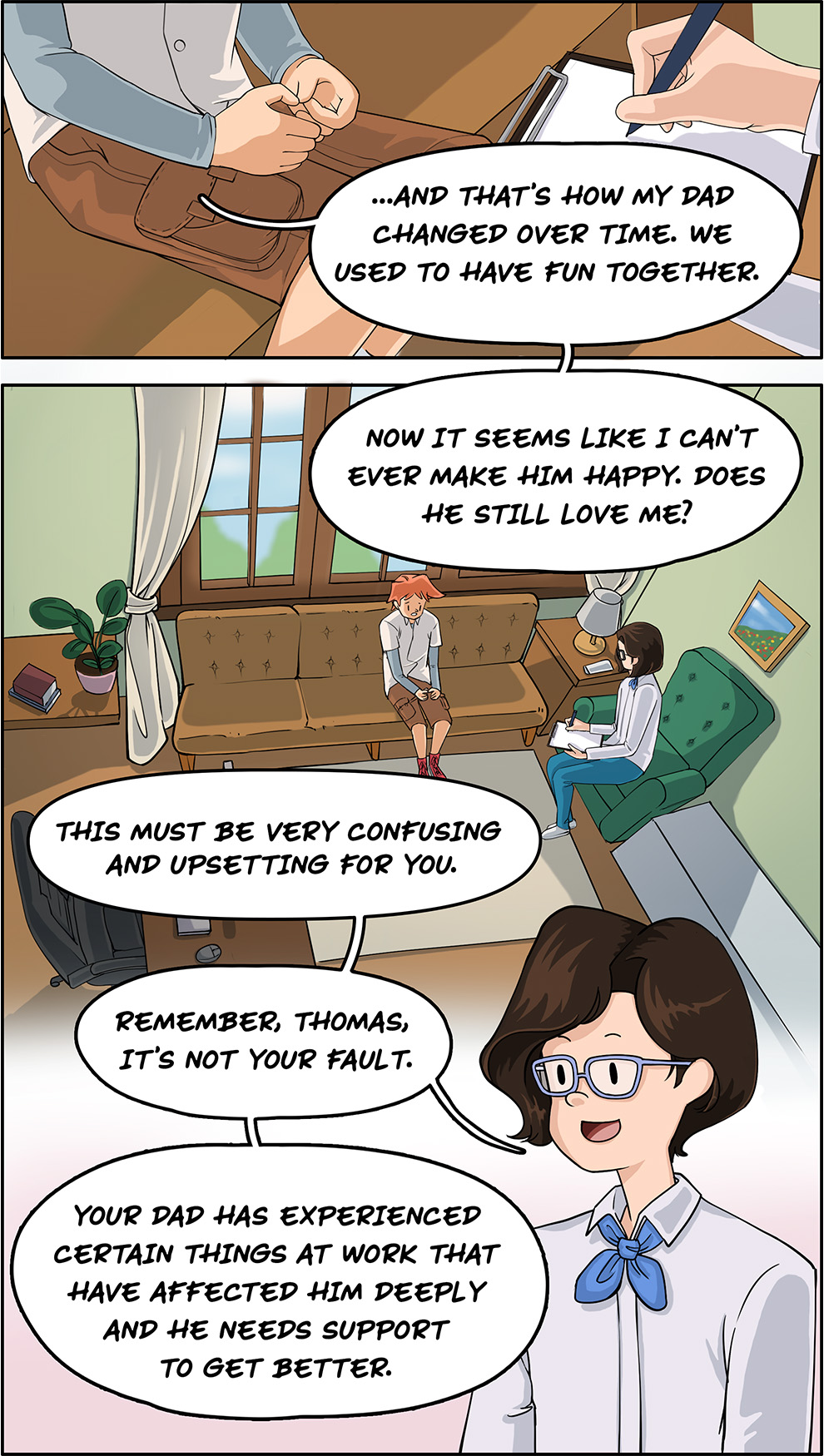
[Thomas sits in Ms. Young’s office.]
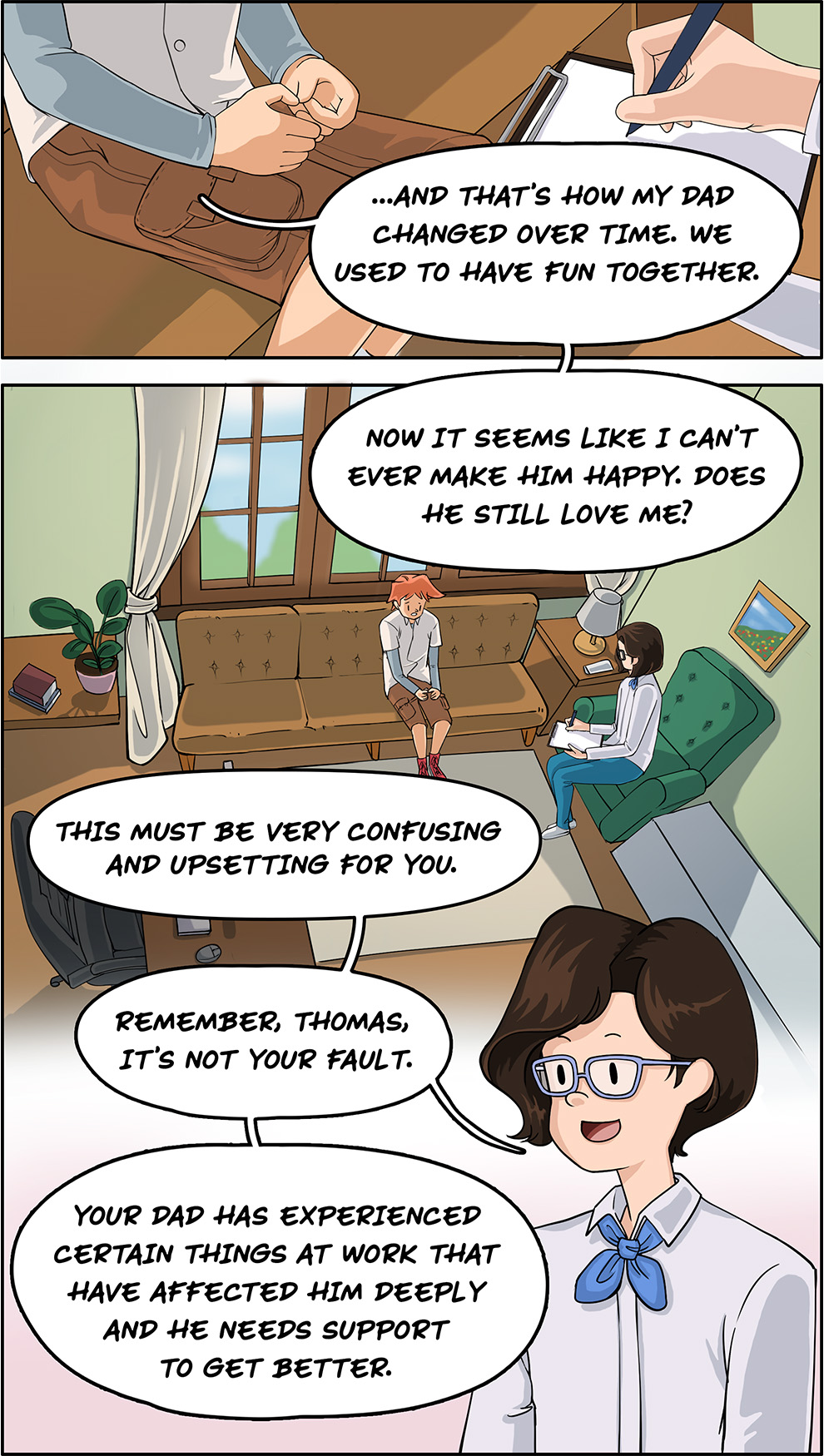
(Thomas): …and that’s how my dad changed over time. We used to have fun together. Now it seems like I can’t ever make him happy. Does he still love me?
(Ms. Young): This must be very confusing and upsetting for you. Remember, Thomas, it’s not your fault. Your dad has experienced certain things at work that have affected him deeply and he needs support to get better. I know about a program where Family members like you can share their experiences and learn more about things like post-traumatic stress injuries.
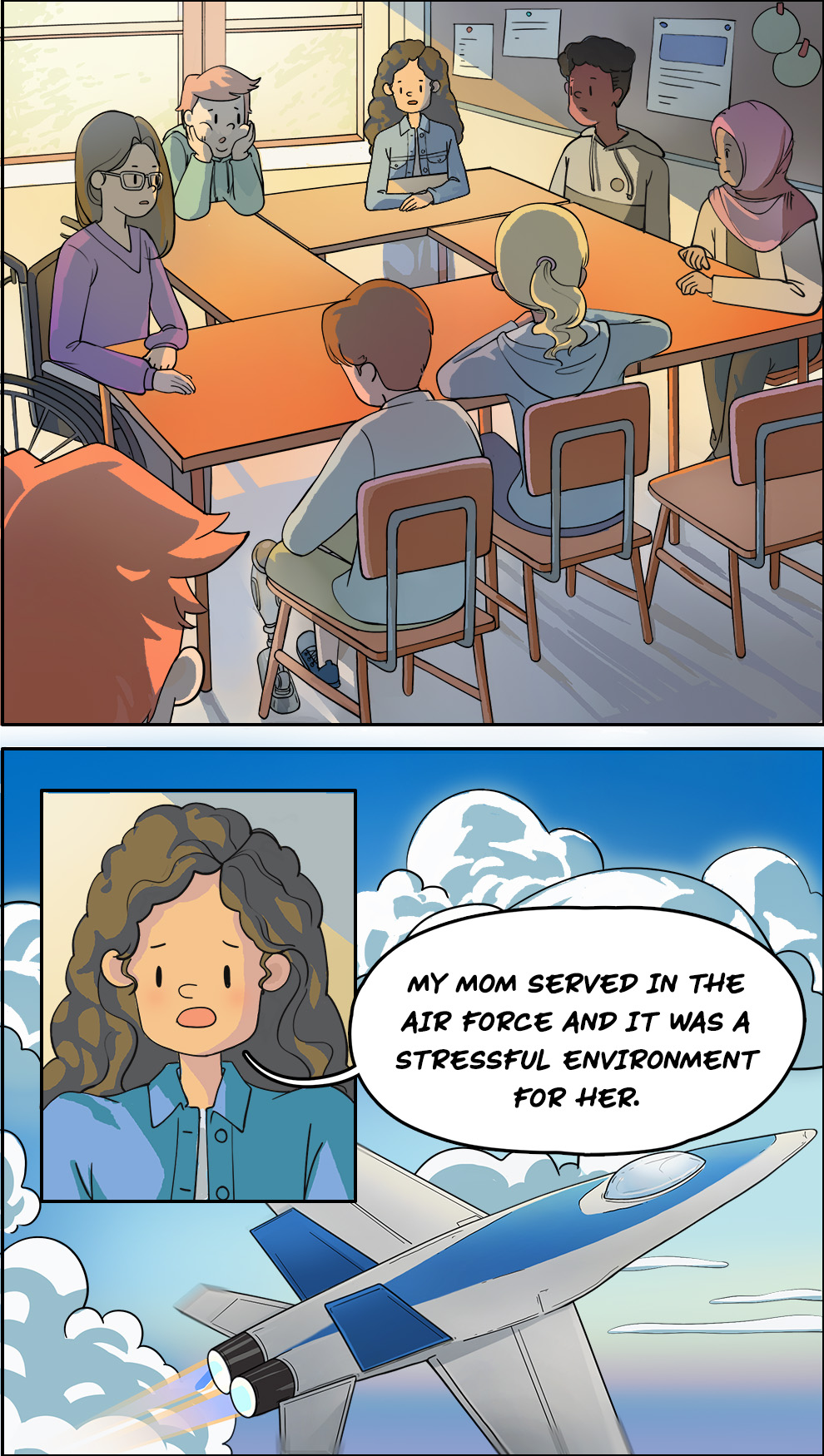
[Thomas arrives at a support session for young Veteran Family members. Two members of the group, Emma and Alex, share their experiences with others.]
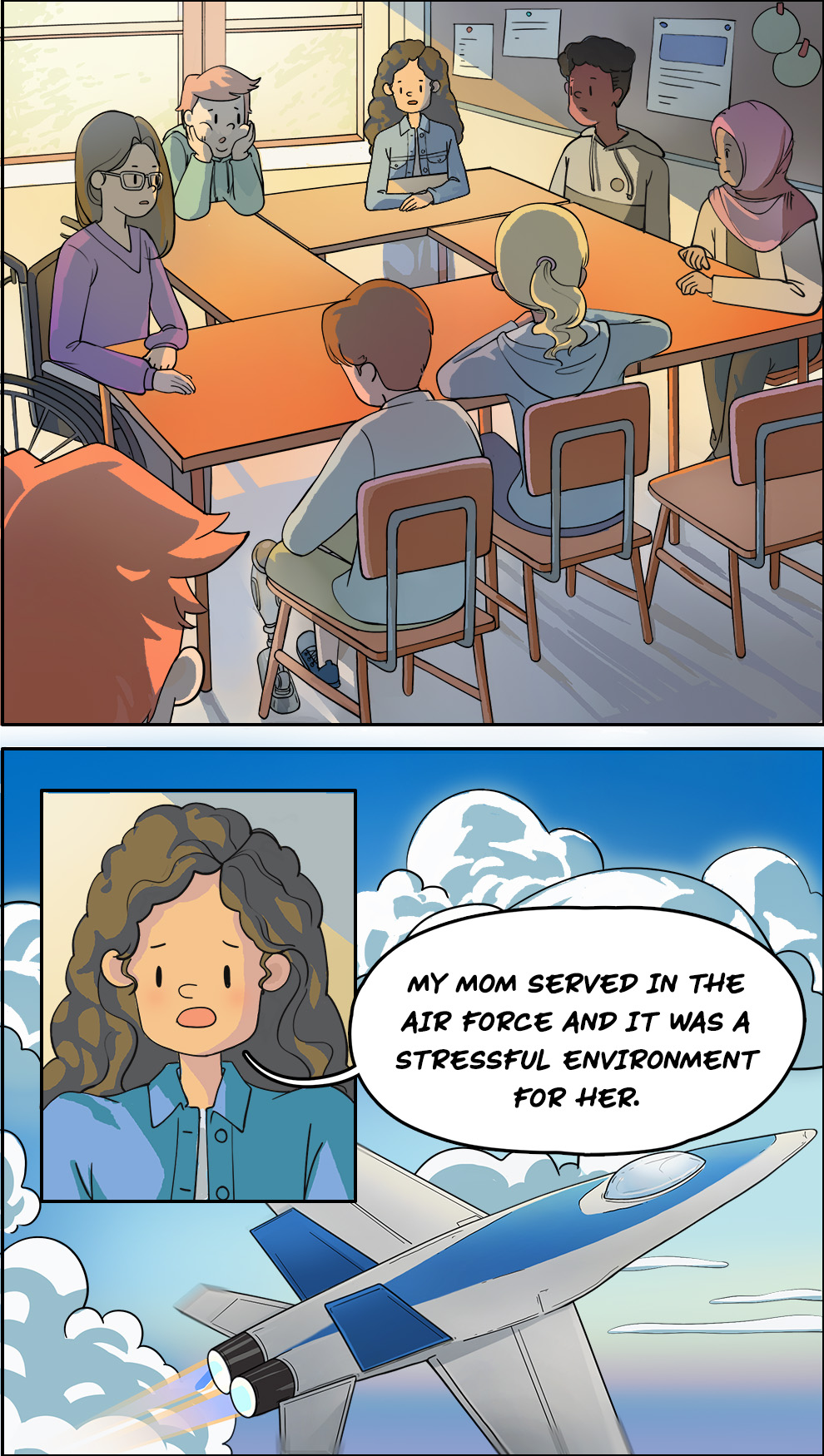
(Emma): My mom served in the Air Force and it was a stressful environment for her. None of us knew what was really going on, but I noticed she was drinking a lot more than usual. My aunt’s in the service too and recommended a therapist. Mom’s getting the help she needs now. I’m here because I need some help too.
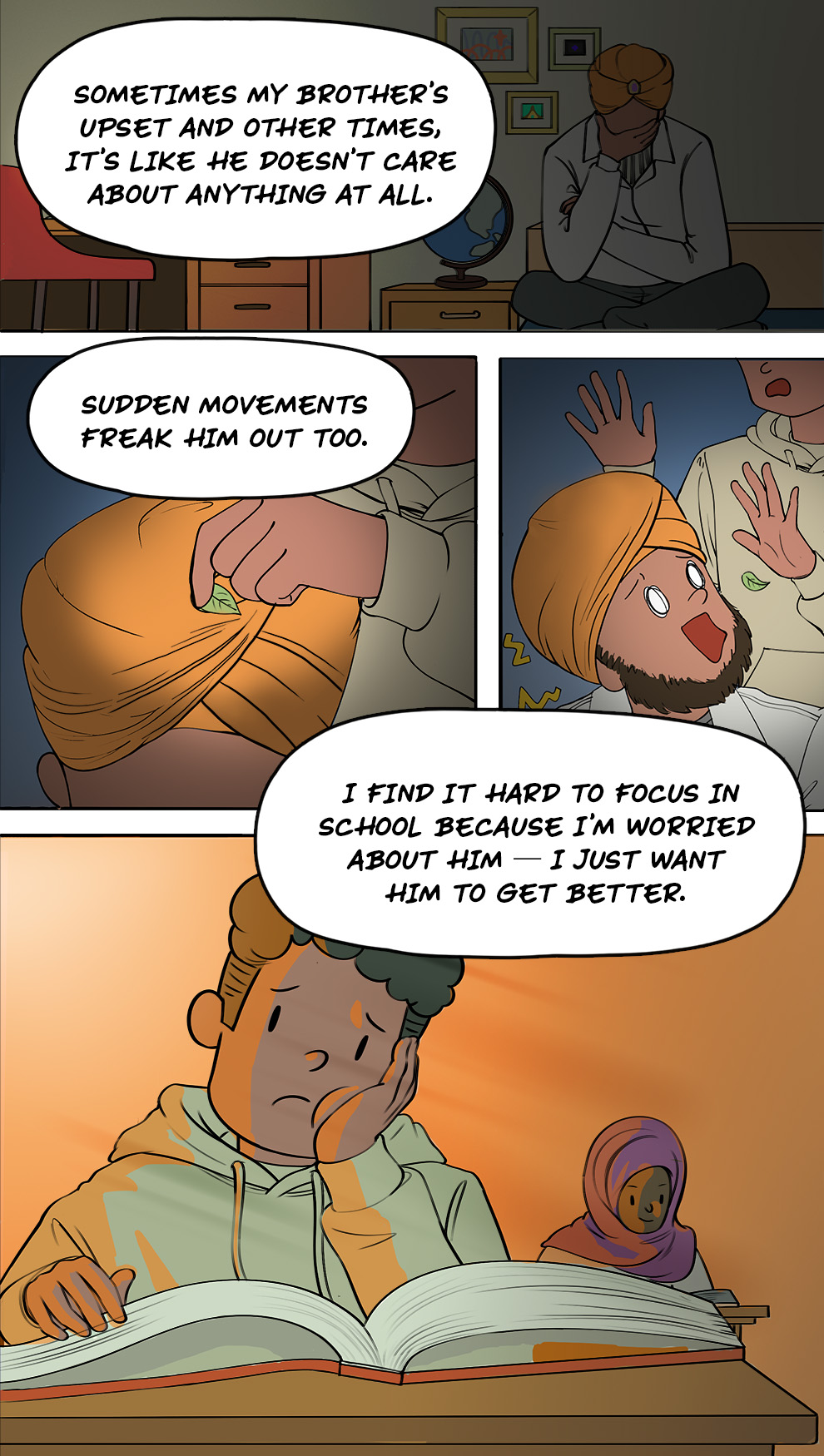
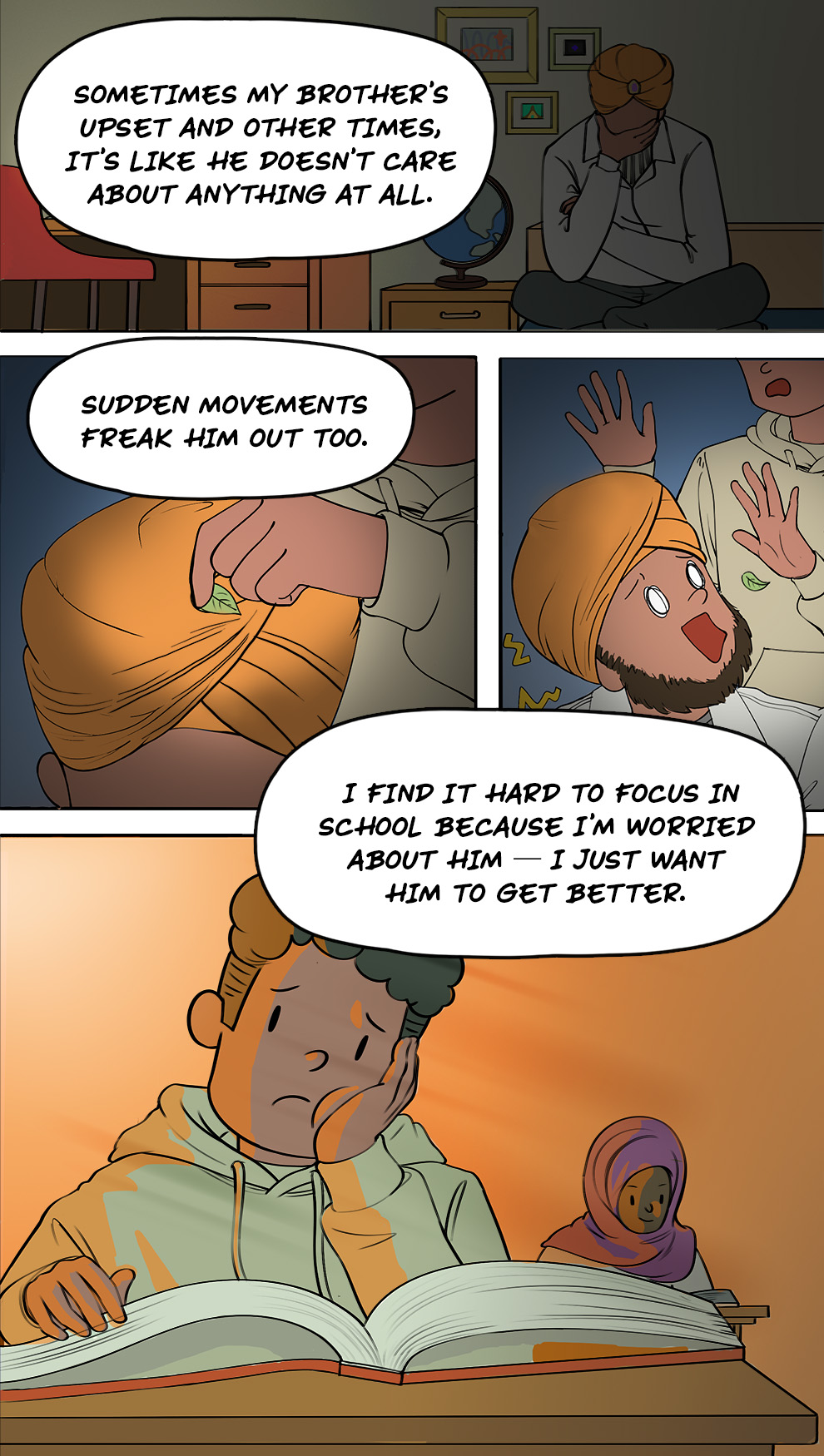
(Alex): My big brother used to be a Mountie. He turns off the TV whenever the news comes on and something bad has happened. I think it reminds him of stuff he’s experienced. Sometimes my brother’s upset and other times, it’s like he doesn’t care about anything at all. Sudden movements freak him out too. I find it hard to focus in school because I’m worried about him — I just want him to get better. It makes my stomach hurt just thinking about it.
[At the end of the session, Thomas receives a key chain with a website URL on it (MindKit.ca).]
CHECK OUT THE REST OF THE COMIC ON THE OTHER TOPIC PAGES TO CONTINUE THE STORY.









[Thomas walks back home. He hesitates for a moment before opening the door.]
(Mom) Thomas, you’re home late. Where were you?
(Thomas) I was doing homework with my friends at school.
[Thomas gently puts down his shoes and school bag. Dad is watching TV in another room.]
[Thomas and his mom are in the kitchen making a snack.]
(Mom) Thomas, can you grab me the sugar from the cupboard, please?
(Thomas) Yeah, sure.
[Thomas grabs the sugar from the cupboard. The cupboard door slams shut loudly: “BANG”]
Thomas cringes and looks over his shoulder towards Dad to check his reaction.
[Dad is startled and jumps up, ready to protect his Family. Dad runs into the kitchen.
(Dad) What was that noise? Is everyone okay?
(Thomas) I’m sorry Dad, it was just the cupboard door slamming.
(Dad): How many times do I have to tell you to keep noise like that down?! It’s not funny!
[Thomas goes to his room. He looks out of the window, thinking back to how Dad has changed.]
[Thomas’s thoughts] I remember Dad waking up in the middle of the night, checking all the doors and windows around the house. Sometimes he wakes up screaming and yelling from nightmares too. Mom’s started sleeping in a different room. We used to go to hockey games together and have picnics at the park, but those things have become too stressful. I feel like I don’t even know him anymore. The look on his face is strange and distant. It seems to be swallowing me whole.
[Thomas sits in Ms. Young’s office.]
(Thomas) … and that’s how my dad changed over time. We used to have fun together. Now it seems like I can’t ever make him happy. Does he still love me?
(Ms. Young) This must be very confusing and upsetting for you. Remember, Thomas, it’s not your fault. Your dad has experienced certain things at work that have affected him deeply and he needs support to get better. I know about a program where Family members like you can share their experiences and learn more about things like posttraumatic stress injuries.
[Thomas arrives at a support session for young Veteran Family members. Two members of the group, Emma and Alex, share their experiences with others.]
(Emma) My mom served in the Air Force and it was a stressful environment for her. None of us knew what was really going on, but I noticed she was drinking a lot more than usual. My aunt’s in the service too and recommended a therapist. Mom’s getting the help she needs now. I’m here because I need some help too.
(Alex) My big brother used to be a Mountie. He turns off the TV whenever the news comes on and something bad has happened. I think it reminds him of stuff he’s experienced. Sometimes my brother’s upset and other times, it’s like he doesn’t care about anything at all. Sudden movements freak him out too. I find it hard to focus in school because I’m worried about him — I just want him to get better. It makes my stomach hurt just thinking about it.
[At the end of the session, Thomas receives a key chain with the MindKit logo on it.]
CHECK OUT THE REST OF THE COMIC ON THE OTHER TOPIC PAGES TO CONTINUE THE STORY.
Understanding the terms
Posttraumatic stress injury
Posttraumatic stress injury (or PTSI for short) is a broad term that refers to any kind of mental health challenge or condition that happens after someone experiences, sees or hears about a traumatic event. You don’t need a diagnosis to have a PTSI.
Operational stress injury
Operational stress injury (or OSI for short) is a more specific term that refers to any kind of mental health challenge or condition that happens after someone experiences, sees or hears about a traumatic event during their job. You don’t need a diagnosis to have an OSI.
Posttraumatic stress disorder
Posttraumatic stress disorder (or PTSD for short) is a specific type of mental health condition that can happen after someone experiences, sees or hears about a traumatic event. PTSD is diagnosed by a licensed medical professional based on specific signs, symptoms and behaviours.
A specific tool is used to diagnose mental health conditions
When it comes to PTSD, the DSM lists four main types of symptoms:
(Narrator) Posttraumatic stress disorder can have four main symptoms.
If your loved one has a posttraumatic stress injury or an operational stress injury, you may see some of these symptoms too.
The first type is re-experiencing.
- Your loved one may have flashbacks during which they feel like they’re back in the traumatic experience.
- These can happen after they’re exposed to certain smells or sounds or even situations that remind them of their trauma.
- You may notice they have trouble focusing or concentrating when you’re together.
The second is avoiding.
- Your loved one may do things to avoid thinking about their traumatic experiences.
- You may notice that activities with big crowds or loud noises, such as the movies, concerts or sporting events, are not enjoyable for them anymore.
- Your loved one might also use alcohol or other things to avoid bad feelings and thoughts.
The third is having negative thoughts or feelings.
- Your loved one may get upset or angry easily.
- They may seem as if they are in a bad mood most of the time or may even stop showing their emotions.
The fourth is being on-edge and reactive.
- Your loved one may have a quick temper or be overly suspicious of things you see as normal.
- You may find them calling or texting a lot to check on you when you are out.
- You may notice that certain things, like sudden movements, bother them.
(click/tap on the tiles to show examples of each symptom)

Re-experiencing events
Re-experiencing events

Avoiding specific activities
and experiences
Avoiding specific activities and experiences

Having negative thoughts
and moods
Having negative thoughts and moods

Being on edge and
reactive most of the time
Being on edge and reactive most of the time
It’s important to reflect on how you’re feeling too
When someone you love has PTSD or experiences a PTSI or an OSI, it can be stressful for you and other Family members. It may feel like a rollercoaster of emotions.
It’s important to know that everyone reacts differently and there is no right way to think, feel or act. Your responses are normal and okay. There may be times when you need to ask for help because things feel so overwhelming or you can’t seem to shake a negative emotion and that’s okay too. There are people and places where you can get helpful tips and strategies to help you feel better.

You may think, feel and act in various ways
Here are some of the ways you may be affected by your loved one’s injury. You may experience some, all or none of these. Check out our written resource on PTSI and you to learn more.
(Click or tap on the tabs to show examples)
- My loved one will never get better
- My Family will never be like it was
- My loved one’s symptoms are my fault
- My Family member doesn’t love me anymore
- Confusion
- Anger
- Embarrassment
- Disappointment
- Sadness
- Hopelessness
- Fear
- Lack of emotions
- Being overly alert
- Having difficulty making or keeping relationships
- Acting older or younger
- Over- or under-achieving
- Avoiding your activities and hobbies
- Doing risky things or acting out
- Harming yourself or having thoughts of suicide
- Eating too much or too little
Your day-to-day life might be different from before
(Narrator) Having a loved one with a mental health condition can be stressful.
You might find it hard to understand what is going on. You might also have thoughts like “my Family will never be like it was” or “it is my fault that they are behaving this way.”
You may experience a rollercoaster of emotions, including confusion, anger, fear, sadness or hopelessness. You may even feel the opposite, as if you are numb.
You may start to act or behave in different ways as well. For example:
- You may not want to hang out with your Family and friends as much as you used to, or find it hard to do your schoolwork or participate in sports or clubs.
- You may try to be on your best behaviour all the time or do extra chores around the house. On the other hand, you may instead start to act out or break rules more.
You may experience physical symptoms, such as headaches or stomach aches.
You may notice these effects right away, but sometimes, it can take time.
It is important to know that everyone reacts differently and there is no right way to think, feel or act. Your responses are normal and okay.
There may be times when you need to ask for help because things are so overwhelming and that’s okay too.
What matters most is that you take steps to look after yourself and your mental health. This could include learning tools or strategies to help you cope or talking to a trusted adult or professional when things feel especially tough.
(Narrator) When someone you love, like your mom or dad, is struggling with their mental health, your day-to-day life might be different from how it was before, especially if they are living with you.
You may find that there is more stress and conflict between your Family members. Things you and your Family used to do may become more stressful.
You may also start doing new tasks or chores to try to support your Family members.
Receiving mental health treatment can create more changes in your life.
- For example, if your loved one is getting help at a hospital or clinic, they might not be home as much or may be away for a long time.
- You and your Family might also go to therapy, either on your own or together as a group.
All these changes can be hard on you, especially at first. Try to always keep in mind these three important things:
- It’s not your fault.
- It’s not your responsibility to “fix” what is happening. There are many different treatment options available for your loved one to support their recovery.
- Your Family member still loves you.
With all of these changes, your day-to-day life might be different from how it was before. These changes may feel stressful, especially at first. Keep in mind that change can lead to positive results, like learning new skills or finding new ways to do things.
Here are some of the ways your life may change:
(click/tap on the tiles to show examples)

Changing routines
Changing routines
- Your usual Family activities may change slightly to make them more PTSI-friendly. For example, instead of going to the movie theatre, you might have movie night at home.
- You or your Family members might go to therapy after school, on your own or together as a group.
- Your loved one might be away from home for a period while they get the help
they need. - You may spend more time doing things with other Family members.

Shifting roles and responsibilities
Shifting roles and responsibilities
- You or your other Family members may take on new tasks that you never did before, like picking up medication or driving to and from appointments.
- You may pick up some additional chores, like cooking dinner or mowing the lawn, to help around the house.
Family functioning
Family functioning
- You may feel like it’s more difficult to communicate with your Family members at times. For example, you might not talk as much as you used to.
- It may feel like you do not get along with your Family as well as before or that there is more conflict.
- Certain activities, like driving to school, may become more stressful and start to feel more like a burden.
- You may start to feel closer to your Family as you adapt to the changes.
Three important things to always keep in mind
- It’s not your fault.
- It’s not your responsibility to “fix” the situation. There are many different treatment and support options available.
- Your Family member still loves you!
